About a month or so ago I was corresponding with the manager of a small PFT lab and in response to one of their questions I had mentioned that there were no CPT codes for MIP/MEP. They responded with 'what's a CPT code?' so I guess this means that CPT codes aren't as well known as I thought they were.
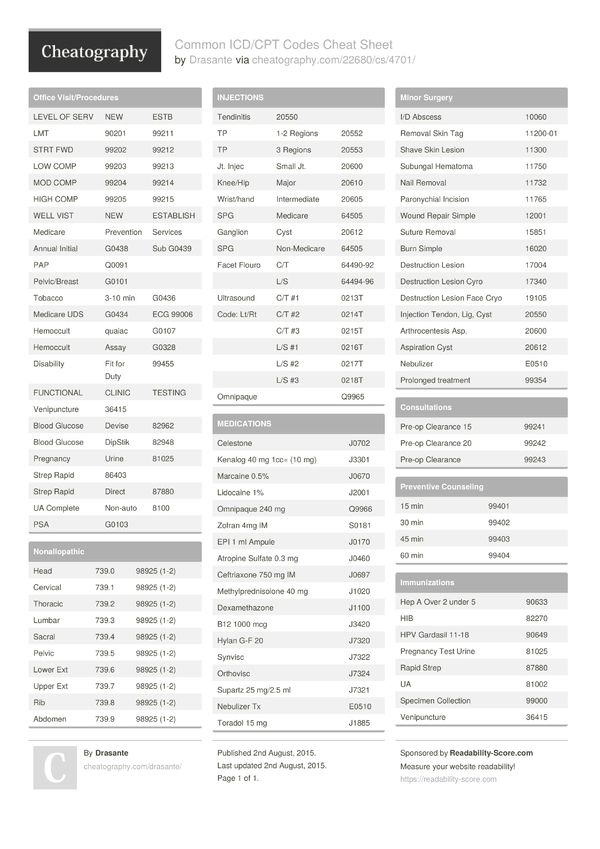
CPT stands for Current Procedural Terminology and is managed by the American Medical Association. CPT codes are a relatively universal way to classify and describe all medical tests and procedures. They are also used by all insurance companies for medical billing so one downside to this is if there isn't a CPT code for a test or a procedure, you can't bill for it. CPT codes also include conditions that limit performing (or at least billing for) some tests in various combinations and to some extent this drives the way PFT tests are ordered and performed.
- CPT 15271 (application of skin substitute graft to, for example, leg or ankle). This code is based on a wound size (after cleansing, prepping, and/or debriding) maximum of 100 sq cm.
- Procedure / Surgical Code Look up CPT CODE SEARCH. Direct or patch closure, sinus venosus, with or without anomalous pulmonary venous drainage.
The CPT codes are reviewed, revised and updated annually. There have been a number of additions and changes to PFT CPT codes during the last five to ten years, and I'd say that with a few notable exceptions, most current PFT testing is adequately covered by the CPT codes. The current PFT CPT codes are:
| CPT: | Description: | Exclusions: |
| 94010 | Spirometry, including graphic record, total and timed vital capacity, expiratory flow measurement(s), with or without maximum voluntary ventilation. | Do not report in conjunction with 94150, 94200, 94375, 94728. |
| 94011 | Measurement of spirometry forced expiratory flows in an infant or child through 2 years of age | |
| 94012 | Measurement of spirometry forced expiratory flows, before and after bronchodilator, in an infant or child through 2 years of age. | |
| 94013 | Measurement of lung volumes (i.e., functional residual capacity (FRC); forced vital capacity (FVC), and expiratory reserve volume (ERV) in an infant or child through 2 years of age. | |
| 94014 | Patient-initiated spirometry recording per 30 day period of time; includes reinforced education, transmission of spirometry tracing, data capture, analysis of transmitted data, periodic recalibration and review and interpretation by a physician or other qualified health professional. | |
| 94015 | [patient-initiated spirometry] recording (includes hook-up, reinforced education, data transmission, data capture, trend analysis, and periodic recalibration). | |
| 94016 | [patient-initiated spirometry] review and interpretation only by a physician or other qualified health professional. | |
| 94060 | Bronchodilator responsiveness, spirometry as in 94010, pre- and post-bronchodilator administration. | Do not report in conjunction with 94150, 94200, 94375, 94728. For prolonged exercise test for bronchospasm with pre- and post-spirometry use 94620. |
| 94070 | Bronchspasm provocation evaluation, multiple spirometric determination s as in 94010, with administered agents (eg. antigen(s), cold air, methacholine). |
| CPT: | Description: | Exclusions: |
| 94150 | Vital capacity, total (separate procedure). | Do not report in conjunction with 94010, 94060, 94728. |
| 94200 | Maximum breathing capacity, maximum voluntary ventilation. | Do not report in conjunction with 94010, 94060. |
| 94250 | Expired gas collection, quantitative, single procedure (separate procedure). | |
| 94375 | Respiratory flow volume loop | Do not report in conjunction with 94010, 94060, 94728. |
| 94400 | Breathing response to CO2 (CO2 response curve). | |
| 94450 | Breathing response to hypoxia (hypoxia response curve). | For high altitude simulation test (HAST) see 94452, 94453. |
| 94452 | High altitude simulation test (HAST) with interpretation and report by a physician or other qualified health professional. | Do not report in conjunction with 94453, 94760, 94761. |
| 94453 | [HAST] with supplemental oxygen titration. | Do not report in conjunction with 94452, 94760, 94761. |
| 94620 | Pulmonary stress test simple (eg. 6-minute walk test, [or] prolonged exercise test with pre- and post- spirometry and oximetry. | |
| 94621 | Pulmonary stress test, complex (including measurement if CO2 production, O2 uptake, and electocardiographic recordings). | |
| 94680 | Oxygen uptake, expired gas analysis, rest and exercise, direct, simple | |
| 94681 | [Oxygen uptake] including CO2 output, percentage oxygen extracted. | |
| 94690 | [Oxygen uptake] rest, indirect (separate procedure). | |
| 94726 | Plethysmography for determination of lung volumes and when performed, airway resistance. | Do not report in conjunction with 94727. |
| 94727 | Gas dilution or washout for determination of lung volumes, and when performed distribution of ventilation and closing volume. | Do not report in conjunction with 94726. |
| 94728 | Airway resistance by impulse oscillometry | Do not report in conjunction with 94010, 94060, 94070, 94375, 94726. |
| 94729 | Diffusing capacity (eg. Carbon monoxide, membrane). | Must be reported in conjunction with 94010, 94060, 94070, 94375, 94726, 94727 or 94728. |
| 94750 | Pulmonary compliance study (eg. Plethysmography, volume and pressure measurements). | |
| 94760 | Noninvasive or pulse oximetry for oxygen saturation, single determination. | |
| 94761 | [Oximetry] multiple determinations (eg. During exercise). | |
| 94762 | [Oximetry] by continuous overnight monitoring (separate procedure). | |
| 94799 | Unlisted pulmonary service or procedure. | |
| 95012 | Nitric oxide expired gas determination. | |
| 95070 | Inhalation bronchial challenge testing (not including necessary pulmonary function tests); with histamine, methacholine or similar compounds. | For pulmonary function tests see 94060, 94070 |
| 95071 | For pulmonary function tests see 94060, 94070 | For pulmonary function tests see 94060, 94070 |
ABG associated CPT codes:
A Bogota bag is a sterile plastic bag used for closure of abdominal wounds. It is generally a sterilized 3-liter (0.66 imp gal; 0.79 U.S. Gal) genitourinary irrigation bag that is sewn to the skin or fascia of the anterior abdominal wall. Over the years, many Bulletin articles have been written about changes in CPT codes and how to correctly code clinical scenarios. These articles are a great resource for surgeons and their billing staff and have been organized in the below tabs by topic for easy access. Abdomen, Stomach, Liver, Gallbladder. Intestines, Rectum, Anus.
| CPT: | Description: |
| 36600 | Arterial puncture, withdrawal of blood for diagnosis |
| 36620 | Arterial catheterization or cannulation for sampling, monitoring or transfusion (separate procedure), percutaneous. |
| 82375 | [Blood] Carboxyhemoglobin, quantitative |
| 82800 | [Blood] gases, pH only |
| 82803 | [Blood] gases, any combination of pH, pCO2, pO2, CO2, HCO3 (including calculated O2 saturation). |
| 82805 | [Blood] with O2 saturation, by direct measurement, except pulse oximetry. |
| 82820 | [Blood] Hemoglobin-oxygen affinity (pO2 for 50% hemoglobin saturation with oxygen). |
Hgb Finger stick CPT codes:
| CPT: | Description: |
| 88738 | Hemoglobin (Hgb), quantitative, transcutaneous. |
| 88740 | Hemoglobin, quantitative, transcutaneous, per day, carboxyhemoglbin |
| 88741 | [Hemoglobin, transcutaneous] methemoglobin. |
There are a number of exclusions for different CPT codes and since a number of CPT codes contain combinations of other CPT codes much of this makes sense. You shouldn't, for example, bill for spirometry (94010) when you're also billing for pre- and post-BD spirometry (94060).
The exclusion for diffusing capacity (94729) however, is unusual in that it requires that a DLCO test be performed along with spirometry (which includes pre & post bronchodilator and challenge tests), lung volumes or impulse oscillometry. To some extent I understand this since the quality of a DLCO test depends on inspired volume (VC from spirometry) and VA (TLC from lung volumes) but I don't quite get the connection with impulse oscillometry.
Interestingly, you can't bill for impulse oscillometry (94728) if you perform any form of spirometry (94010, 94060, 94070, 94375) or plethysmography (94726). I can see why this might be the case for plethysmography since that CPT code includes airway resistance measurements (RAW) which could be considered a duplication, but it's not as clear why any form of spirometry would be a duplication as well.
You can bill for an SVC (94150) or an MVV (94200) if they are performed by themselves but if you perform plain spirometry (94010) along with an SVC or an MVV you will only be reimbursed for the spirometry.
On the other hand, for a methacholine challenge test you can bill using both 94070 (spirometry testing) and 95070 (administration of methacholine). Similarly a cold air challenge (and probably a Eucapnic Voluntary Hyperventilation Challenge) could be billed using 94070 (spirometry) and 95071 (administration).
Based on some correspondence I've had in the past, there is a bit of confusion regarding 94620. The wording for this code could have been clearer since it used for either for a 6-minute walk test or for a simple exercise test (usually a bronchspasm evaluation for EIB) with pre- and post-exercise spirometry. Unfortunately 94620 has been read by a number of people as saying that a 6-minute walk test requires pre- and post-spirometry and for this reason I don't know why separate CPT codes weren't assigned to the 6-minute walk and the exercise challenge test.
There are a number of common pulmonary function tests however, that have no CPT code or cannot be billed because of exclusions. Most notoriously, as already mentioned, there is no CPT code for MIP or MEP and the best you can do is to charge it under 94799 (unlisted pulmonary service or procedure). This is hard to understand given that the ATS released standards for respiratory muscle testing in 2002 and that MIP and MEP were a significant part of that, but despite this there is still no CPT code for respiratory pressure measurements (MIP, MEP, NIF and SNIP).
There is also no CPT code for upright and supine spirometry. For that matter, if you perform a complex CPET (94621) pre- and post-exercise spirometry is not included with that CPT code (even though it is for 94620) but you can only bill for simple spirometry (94010).
There are a couple of somewhat leading edge tests for which equipment is being sold that have no CPT codes. Admittedly some of these tests could be considered to be more in the research arena than in clinical testing, but the lack of a CPT code is also an impediment towards the widespread adoption of the tests, even when they have been shown to be clinically useful.

As an example, even though the ERS/ATS has released standards for DLNO testing you can bill for it using the diffusing capacity CPT code (94729) only if you simultaneously perform a DLCO since the code explicitly mentions carbon monoxide and not nitric oxide. This also means that despite the extra cost of performing combined DLCO and DLNO testing, you really aren't able to bill for it.
If you wanted to perform Lung Clearance Index (LCI) testing you would probably be able use 94727 (gas dilution or washout for determination of lung volumes) because it includes the phrase '… and when performed, distribution of ventilation …' and because FRC is also measured (although not TLC and RV) as part of the test. But that means that if you use this code for LCI you can't bill for separate lung volume measurement even if you do so by plethysmograph (94726).
You couldn't however, use 94727 if you wanted to perform a dual-tracer gas single breath washout (DTG-SBW) or a Closing Volume (for the phase III slope) since there is no lung volume measurement included in these tests and that is a required part of 94727.
Overall the CPT codes work relatively well for most common PFT testing situation but I still have a couple concerns. First, some of the descriptions are either ambiguous, poorly worded or rely on somewhat outdated terminology which makes it difficult at times to determine how the codes should be applied to certain situations.
Second, CPT codes are acting as an arbiter forwhich tests can be performed. A particular example is the lack of CPT codes for MIP/MEP as well as other tests that are in the process of advancing into routine clinical testing, such as DLNO, LCI and DTG-SBW. There are ATS/ERS standardization statements that have touched on most of these tests (MIP/MEP 2002, LCI 2013, DLNO 2017) but realistically it is the presence or absence of CPT codes that is determining what is and isn't clinically relevant.
Third, CPT codes are also acting as an arbiter about how testing is performed. Although I understand and in general agree with many of the exclusions, they also limit what tests can be performed within a single testing session. There are likely legitimate clinical reasons why you'd want to perform impulse oscillometry (for airway resistance) and plethysmography (for lung volumes) but the exclusions for 94726 and 94728limits reimbursement if they are performed in the same day.
CPT exclusions can also be a dis-incentive towards performing more comprehensive patient testing. SVC testing should be performed as part of routine spirometry whenever there is any question that the FVC is being underestimated but if you do this you have to accept that you won't be reimbursed for the extra time and effort. Ditto for upright and supine spirometry. Ditto for post-exercise spirometry for CPETs.
To its credit, the procedure for revising CPT codes is a consensus-based, evidence-driven process. But this also means that it is often slow and requires a significant time commitment for anybody requesting a change. Instructions for requesting an update to the CPT codes are on the AMA website (Applying for CPT codes). Notably, the application for requesting a new code or a revision of an older code is about 20 pages long and more than somewhat formidable in that it requires extensive knowledge and documentation concerning the subject in question.
CPT codes are a fact of life and if they didn't already exist we'd probably re-invent them sooner rather than later. Since the way we are reimbursed for testing is determined by CPT codes and their exclusions we generally have to work within the framework they have created. This doesn't mean that they are always right however, nor should they be taken as the final word about what is clinically relevant.
References:
Abraham M et al. Current Procedural Terminology CPT 2015. Published by the American Medical Association, 2014.
ATS/ERS statement on respiratory muscle testing. Amer J Respir Crit Care Med 2002; 166(4): 518-624.
Birnbaum, S. Pulse oximetry. Identifying its applications, coding and reimbursement. Chest 2009; 135(3): 838-841.
Flesch JD, Dine CJ. Lung volumes. Measurement, clinical use and coding. Chest 2012; 142(2): 506-510.
Lange NE, Mulholland M, Kreider ME. Spirometry. Don't blow it! Chest 2009; 136(2): 608-614.
As an example, even though the ERS/ATS has released standards for DLNO testing you can bill for it using the diffusing capacity CPT code (94729) only if you simultaneously perform a DLCO since the code explicitly mentions carbon monoxide and not nitric oxide. This also means that despite the extra cost of performing combined DLCO and DLNO testing, you really aren't able to bill for it.
If you wanted to perform Lung Clearance Index (LCI) testing you would probably be able use 94727 (gas dilution or washout for determination of lung volumes) because it includes the phrase '… and when performed, distribution of ventilation …' and because FRC is also measured (although not TLC and RV) as part of the test. But that means that if you use this code for LCI you can't bill for separate lung volume measurement even if you do so by plethysmograph (94726).
You couldn't however, use 94727 if you wanted to perform a dual-tracer gas single breath washout (DTG-SBW) or a Closing Volume (for the phase III slope) since there is no lung volume measurement included in these tests and that is a required part of 94727.
Overall the CPT codes work relatively well for most common PFT testing situation but I still have a couple concerns. First, some of the descriptions are either ambiguous, poorly worded or rely on somewhat outdated terminology which makes it difficult at times to determine how the codes should be applied to certain situations.
Second, CPT codes are acting as an arbiter forwhich tests can be performed. A particular example is the lack of CPT codes for MIP/MEP as well as other tests that are in the process of advancing into routine clinical testing, such as DLNO, LCI and DTG-SBW. There are ATS/ERS standardization statements that have touched on most of these tests (MIP/MEP 2002, LCI 2013, DLNO 2017) but realistically it is the presence or absence of CPT codes that is determining what is and isn't clinically relevant.
Third, CPT codes are also acting as an arbiter about how testing is performed. Although I understand and in general agree with many of the exclusions, they also limit what tests can be performed within a single testing session. There are likely legitimate clinical reasons why you'd want to perform impulse oscillometry (for airway resistance) and plethysmography (for lung volumes) but the exclusions for 94726 and 94728limits reimbursement if they are performed in the same day.
CPT exclusions can also be a dis-incentive towards performing more comprehensive patient testing. SVC testing should be performed as part of routine spirometry whenever there is any question that the FVC is being underestimated but if you do this you have to accept that you won't be reimbursed for the extra time and effort. Ditto for upright and supine spirometry. Ditto for post-exercise spirometry for CPETs.
To its credit, the procedure for revising CPT codes is a consensus-based, evidence-driven process. But this also means that it is often slow and requires a significant time commitment for anybody requesting a change. Instructions for requesting an update to the CPT codes are on the AMA website (Applying for CPT codes). Notably, the application for requesting a new code or a revision of an older code is about 20 pages long and more than somewhat formidable in that it requires extensive knowledge and documentation concerning the subject in question.
CPT codes are a fact of life and if they didn't already exist we'd probably re-invent them sooner rather than later. Since the way we are reimbursed for testing is determined by CPT codes and their exclusions we generally have to work within the framework they have created. This doesn't mean that they are always right however, nor should they be taken as the final word about what is clinically relevant.
References:
Abraham M et al. Current Procedural Terminology CPT 2015. Published by the American Medical Association, 2014.
ATS/ERS statement on respiratory muscle testing. Amer J Respir Crit Care Med 2002; 166(4): 518-624.
Birnbaum, S. Pulse oximetry. Identifying its applications, coding and reimbursement. Chest 2009; 135(3): 838-841.
Flesch JD, Dine CJ. Lung volumes. Measurement, clinical use and coding. Chest 2012; 142(2): 506-510.
Lange NE, Mulholland M, Kreider ME. Spirometry. Don't blow it! Chest 2009; 136(2): 608-614.
Robinson PD et al. ERS/ATS consensus statement. Consensus statement for inert gas washout measurement using multiple- and single-breath tests. Eur Respir J 2013; 41(3): 507-522.
Salzman, SH. The 6-min walk test. Clinical and research role, technique, coding and reimbursement. Chest 2009; 135(5): 1345-1352.
Zavorsky GS et al. Standardisation and application of the nitric oxide single-breath determination of nitric oxide uptake in the lung. Eur Respir J 2017; 49: n1600962.
PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
Here's how to decode the code on a Hershey's wrapper. Hershey uses a two digit alpha-numeric code to denote the month and year of the expiration date. Here's what the Hershey's site says:
There is an ink stamped code on Hershey's products. Within that code, usually at the end, there is a two character code that represents the year and the month until which the product is expected to be within its peak freshness. The first character is a number, (0-9) that represents the year. The second character is a letter, (A-L) that represents the month. A=Jan., B=Feb., etc. For example, a code of 7D is best before until April 2007.
My Hershey's Twosomes Almond Joy (Limited Edition) bar has a code that's on two lines:
1BE
7C K2
I'm guessing the 7C is the one I want, so that means that the bar is considered fresh until March 2007.
My York Peppermint Patties:
13NYU
6K
This would expire in November 2006, so I got in just under the wire.
A Heath bar:
14HR2
D 6L
This one would expire in December 2006. Just remember, L is the LAST month!
Related Candies
Whitman Patch Cpt Codes
POSTED BY Cybele AT 10:20 am Candy • Expiration Codes • Hershey's • News •

